Heat related illnesses

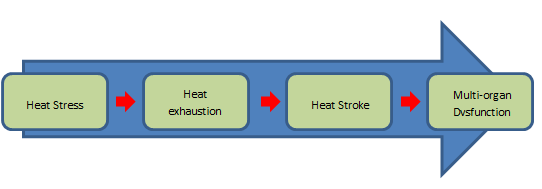
Following last week’s warm weather and in advance of more of the same, it is important to identify the difference between heat stress, heat exhaustion and heat stroke.
Heat related illness is a continuum of heat related conditions; it can be exogenous, caused by environmental factors (e.g the sun) or endogenous (e.g drugs and exercise). It is a relatively uncommon presenting condition but can be life threatening and it is estimated that there are around 2000 deaths in the UK annually (Hijat et al, 2014).
In heat illness there is an imbalance in the metabolic production and subsequent loss of heat by the body. This increase in core body temperature has a number of undesirable effects on many body systems and systemically leads to swelling and degeneration at both cellular and tissue level. The cellular changes at increased temperatures causes cellular organelles to swell and stop functioning properly. Cell membranes become distorted, leading to an unwanted increase in permeability and inappropriate movement of ions into and out of the cells. Red blood cells can also change shape at elevated temperatures and their capacity to carry oxygen is deceased. At higher temperatures cells will also undergo inappropriate apoptosis and die.
It is important that all conditions are managed adequately to prevent minor conditions progressing to the more serious.
Heat stress
This is a mild form of heat illness, it can be self-managed, but if left untreated can progress to more serious conditions.
Features of heat stress:
- temperature – normal or mildly elevated
- heat oedema – swelling of the feet and ankles
- heat syncope – vasodilation and dehydration causing hypotension
- heat cramps – sodium depletion causing cramps.
Heat exhaustion
Without any management of the symptoms (and removing the cause), heat stress can rapidly progress to the more serious heat exhaustion. Whilst less severe than heat stroke, patients will present as being acutely unwell. The deterioration to this state is caused by excess fluid loss due to continued sweating, and electrolyte imbalance. This is often seen after prolonged exposure to heat, usually over hours to days. The patient’s body temperature is likely to rise above 37oC but will be below 40oC.
Features of heat exhaustion:
- systemic reaction to prolonged heat exposure (hours to days)
- temperature - >37°C and <40°C
- headache, dizziness, nausea, vomiting, tachycardia
- hypotension, sweating, muscle pain, weakness and cramps
- haemoconcentration
- hyponatraemia or hypernatraemia
- may progress rapidly to heat stroke.
Without treatment a further rapid deterioration can occur resulting in heat stroke.
Heat stroke
Heat stroke is a life-threatening emergency with a mortality rate of up to 50%. It is a systemic inflammatory response to a core body temperature >40.6°C, in addition to a change in mental status and organ dysfunction. There are two types of heat stroke.
Non-exertion heat stroke is due to very high external temperatures and/or high humidity; it tends to occur in the elderly, very young or the chronically ill.
Exertional heat stroke is due to excess heat production and tends to occur in athletes including marathon and endurance runners, manual workers, fire-fighters and military personnel.
Features of heat stroke:
- core temperature >40°C
- hot dry skin (sweating is present in about 50% of cases of exertional heat stroke)
- early signs and symptoms e.g extreme fatigue, headache, fainting, facial flushing, vomiting and diarrhoea
- cardiovascular dysfunction including seizures and coma
- liver and renal failure
- coagulopathy
- rhabdomyolysis.
Recovery from heat stroke even after appropriate treatment and rehabilitation may be incomplete and leave patients with persistent functional impairment. The systemic effects of heat stroke can lead to a variety of life threatening systemic conditions including:
- disseminated intravascular coagulation
- rhabdomyolysis
- renal failure
- hepatic necrosis
- metabolic acidosis
- decreased tissue perfusion
- cerebral and cerebellar damage.
For the less severe cases of heat stress and exhaustion the removal of clothing, placing the patient in a cool environment away from the heat source, rehydration and cooling by fanning and water misting, should be sufficient to reverse the effects of the cause. Be sure to monitor the patient’s temperature throughout treatment to ensure hypothermia is not induced.
The above techniques can be used for patients suffering with heat stroke also. However, there should be no delay on scene in order to commence this treatment.
As with any patient suffering with a life-threatening condition, management of any ABC problems should be your priority before commencing a blue light transfer, with pre-alert, to the emergency department. If the patient has an indication for oxygen (to maintain SpO2 >94%) then deliver immediately. If the patient has an indication for fluid therapy, this can be administered but must be completed en route so as not delay transport.
Ice packs can be applied to the patient’s neck, axilla and groin, if available, and must be wrapped in a thin cloth to prevent frostbite. Ensure that the air conditioning is on full, or the windows open, whilst in transit.
Normal monitoring should be in place (ECG, observations and blood glucose) and should be continued throughout your transport.
Published 9th July 2015