When responding to a female of childbearing age where the nature of the call is suggestive that a baby has been delivered, the following actions must be taken by the crew on arrival at the property:
|
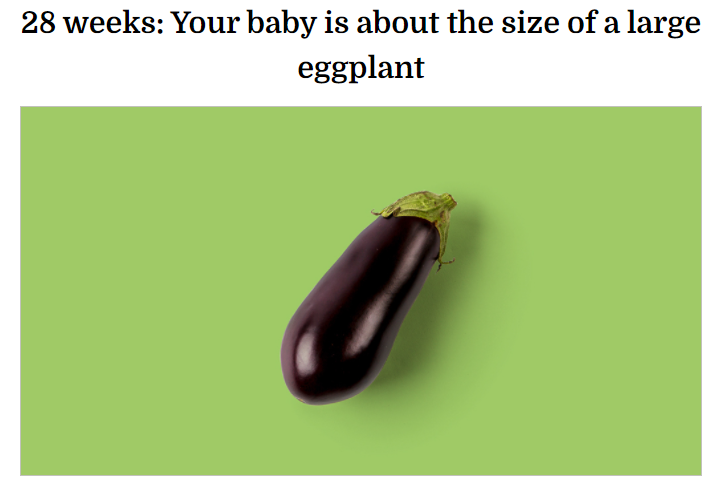
If known or suspected 24 or more weeks of gestation |
Resuscitate and rapidly transport to hospital |
|
If known or suspected less than 24 weeks of gestation with signs of life |
Support signs of life and rapidly transport to hospital |
|
If known or suspected less than 24 weeks gestation with no signs of life |
Arrange dignity and support for mother and family members and convey mother and foetus to hospital |
Assessing for signs of life MUST include auscultation of heart sounds alongside assessment of the baby’s primary survey.
Nature of calls which may indicate delivery (list not exhaustive): PV bleed, miscarriage, pre-term delivery, delivery, birth, labour, obstetric emergency
Exceptions: signs unequivocally associated with death - foetal maceration (when the child is still born and died more than a day before birth as indicated by the skin loosening and sloughing off when touched).
Regardless of resuscitation decisions, all foetal tissue must be conveyed to hospital. This should be done in a dignified manner using a cuddle pocket for a foetus who shows no signs of life.
Please see JRCALC/clinical manual app/emergency birth in the community cards for further reference.
If you have any further concerns, please contact your LOM for assistance.
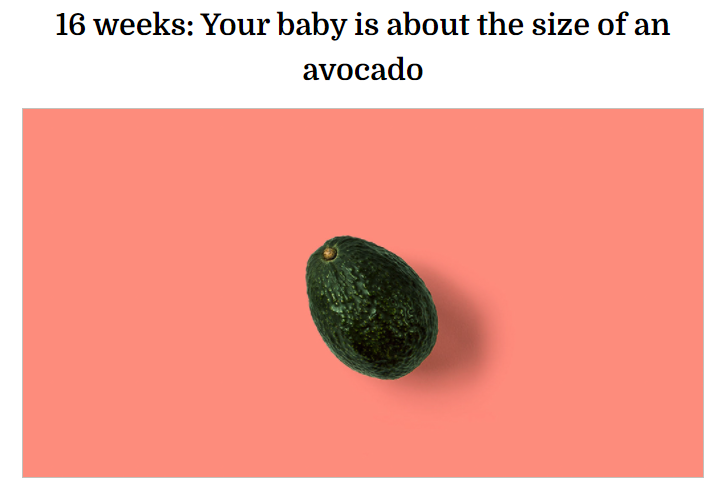
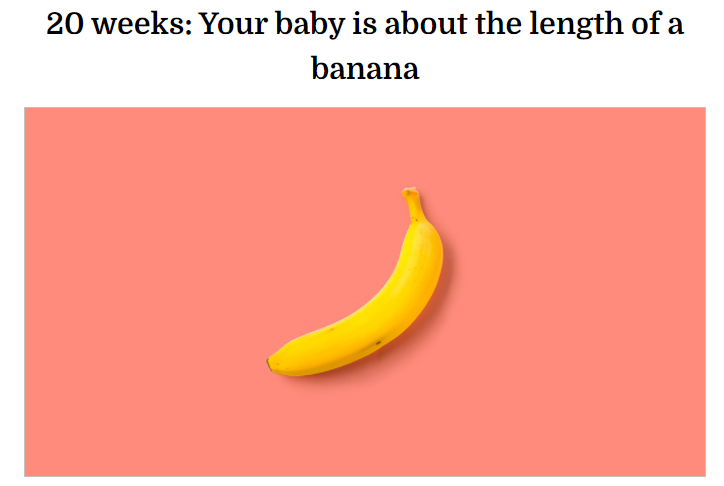
Appendix 1 – Approximate Size of Baby by Gestational Age